Neurosurgeons

Tipu Aziz
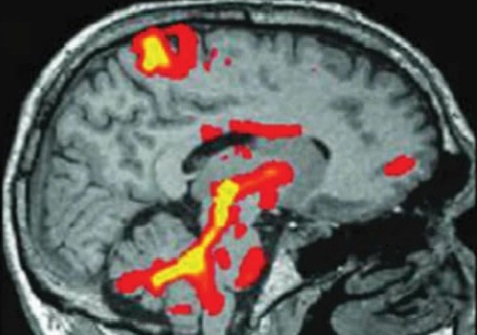
Professor Aziz first became interested in surgical treatments for Parkinson's disease as a neurophysiology student in the 1970s. Ironically, by the time he had qualified as a neurosurgeon, the development of levodopa had resulted in surgery for Parkinson's disease being more or less abandoned. However by the late 1980s it was apparent that after years of treatment with levodopa patients developed crippling side effects such as profound motor fluctuations and severe writhing movements that could be as bad as the untreated disease, and there was renewed surgical interest.
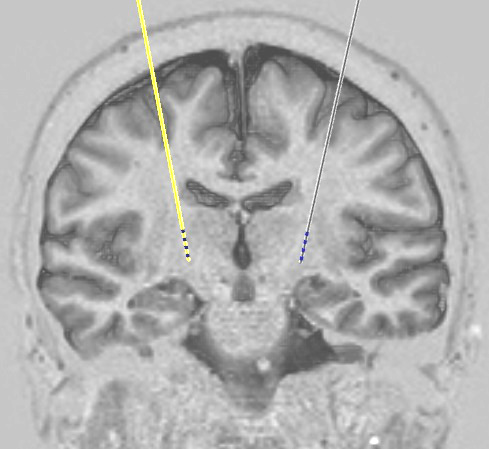
Professor Aziz has played a pivotal role in the development of two of the Deep Brain Stimulation targets used in PD, the subthalamic nucleus (STN) and the pedunculopontine nucleus (PPN). He pioneered DBS for dystonia and multiple sclerosis, and established Oxford as a major international centre for surgery for movement disorders. In 1999 he started performing DBS for neuropathic pain, in which Oxford now has more experience than any other centre in the world. He is the author of over 200 scientific publications and in 2013 was elected Fellow of the Academy of Medical Sciences. NDSS web page

Alexander Green
Alex Green obtained a first class honours degree in Neuroscience in 1994 at University College London, then read medicine, graduating in 1997. He trained in Neurosurgery at St Bartholomew's and the Royal London hospitals, and then Oxford where he was a National Institute of Health Research (NIHR) Academic Clinical Lecturer. He was appointed Spalding Senior Lecturer in neurosurgery at the University of Oxford in 2009.
Mr Green's research focuses on the effects of deep brain stimulation and other forms of neuromodulation on the autonomic nervous system, the part of the nervous system that controls unconscious and automatic functions such as breathing, heart rate, blood pressure, and bladder control. This work has won awards from the Congress of Neurological Surgeons, Royal Society of Medicine, and International Neuromodulation Society. He is currently an examiner in Principles of Clinical Anatomy for the University of Oxford, Training Programme Director for Neurosurgery in the Thames Valley and he sits on a number of research trial committees including a data monitoring committee, steering committee and clinical advisory board. NDSS web page
James FitzGerald
James FitzGerald studied Physics at Oxford University, graduating in 1992, then medicine, also at Oxford, graduating in 1998. After obtaining a PhD in neuroelectronic interfacing at Cambridge University he returned to Oxford to take up a Consultant position in 2012.
Dr FitzGerald works on implanted electronic devices that interface directly with parts of the nervous system. At present his main focus is on the development of a novel type of interface capable of recording signals from motor axons in severed peripheral nerves after amputation, with the aim of using these signals to control advanced prosthetic limbs. This requires advances in several areas including polymer microfabrication techniques, microsurgical implantation methods, and the development of multichannel signal processing and pattern recognition algorithms. A further problem is that like virtually all surgical implants, interfaces evoke a foreign body response that leads to the deposition of scar tissue on their surfaces, which leads to gradual electrical failure of the device. A major strand of his work at present concerns the development of techniques for long term scar suppression. NDSS web page

Stana Bojanic
Neurologists

Marko Bogdanovic

Binith Cheeran
Dr Binith Cheeran completed his PhD at the Sobell Department of Movement Disorders and Motor Neurophysiology at the Institute of Neurology, London. He was appointed as a Senior Clinical Fellow at the University of Oxford in 2013. He specializes in Parkinson’s Disease and other Movement Disorders.
Dr Cheeran’s research has been focussed on Transcranial Magnetic Stimulation (TMS) technology which allows neuroscientists to non-invasively study brain function, and motor control in particular, with a high degree of temporal and spatial specificity. Moreover, as several TMS paradigms can modulate underlying cortical activity, there is considerable interest in employing these paradigms as part of therapeutic or restorative therapy. Dr Cheeran has been working to improve our understanding of this valuable research tool and its applications in the field of Parkinson’s Disease. NDCN web page
Nurse specialists - movement disorders

Beth Forrow

Claire Fletcher

Pedro Rebelo
Nurse specialists - pain neuromodulation

Liz Moir

Karen Dawson

Rodrigo Ortega

Clare Camidge
Clinical lecturer

Martin Gillies
Research Fellows

Sandra Boccard
DPhil students

Dali Wu

Holly Roy

Laurie Pycroft
PAs

Vicky Ford
Copyright OFN Wednesday, 10 August, 2016.