Occipital nerve stimulation
Occipital nerve stimulation (ONS) is used to treat severe migraine or cluster headaches that have not responded to conventional treatments. ONS involves electrically stimulating the greater occipital nerves (GON), which are a pair of nerves (one on each side) that run under the scalp from the back of the neck upwards towards the top of the head. It has been found that by stimulating these nerves the frequency and intensity of headaches can in successful cases be reduced. It is important to note that it is not usually possible to completely stop all attacks this way and other treatments may well need to be continued alongside ONS.
What is an ONS system made up of?
The system consists of two components:
- A pair of electrode wires that are inserted underneath the scalp
- An implanted pulse generator (IPG), which is a small box that contains a battery and circuitry to produce the stimulus current
 An electrode for ONS *
An electrode for ONS *The electrode
This is shaped like a straight wire. There are several electrical contacts on the shaft of the wire to deliver the electrical pulses.
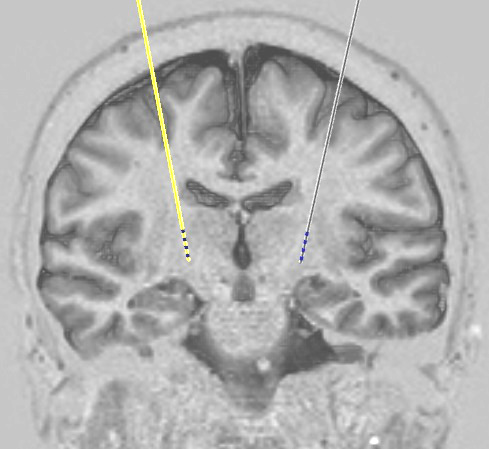
The implanted pulse generator (IPG)
This is commonly referred to as the 'battery' but it also contains the circuitry that produces the small electrical current that is sent to the contacts on the electrode. The IPG is usually implanted under the skin below the collar bone.
Two types of IPG are available:
- Rechargeable
- Non-rechargeable
For a description of the pros and cons of each type and how we choose between them, see our page on IPG types. For most patients we recommend a rechargeable IPG.
How is it implanted?
The operation is performed under general anaesthesia. A small incision is made in the scalp on the back of the head, and the two electrode wires are passed through it to lie under the scalp, one on each side, so as to be in a position to stimulate both left and right GONs. Wires running from these electrodes are passed under the skin to a second incision which is made usually below the left collar bone. Here, the wires are attached to the IPG, which is then placed under the skin. We then run electrical tests on the system to make sure all the parts and connections are working properly.
After surgery
It is usually possible to go home the day after surgery. Patients return two weeks later to have sutures removed, and the system is switched on at that point.
The benefits of ONS may take time to develop, and a lack of immediate improvement after switching the system on should not be interpreted as failure of the treatment. Advice will be given to patients regarding the continuation of any painkilling medications they are on before surgery. In general, even if ONS is very effective, it is best to reduce these gradually rather than stop them abruptly.
Any problems
If there are any problems with a system that we have implanted, please contact us. Patients are always given the contact details of one of our specialist nurses who should be the first port of call. They are available every weekday during working hours to talk to patients, relatives, or their general practitioners. In the event of an emergency occurring out of hours, advice should be sought from the on-call neurosurgical service at the John Radcliffe Hospital in Oxford.
The commonest complication with neuromodulation systems is infection which occurs in around 1 case in 20. The most likely time for this to appear is within the first few weeks to months after implantation of a new system or replacement of an old battery or pump. If there are any concerns about the appearance of a wound or any other symptom that might suggest infection, CALL US. If you are a patient then for this specific issue please call us rather than your GP. If you are a GP then please do not attempt to treat a possible wound infection with antibiotics but call us instead.
* Image courtesy of Medtronic
Copyright OFN Wednesday, 11 February, 2015.